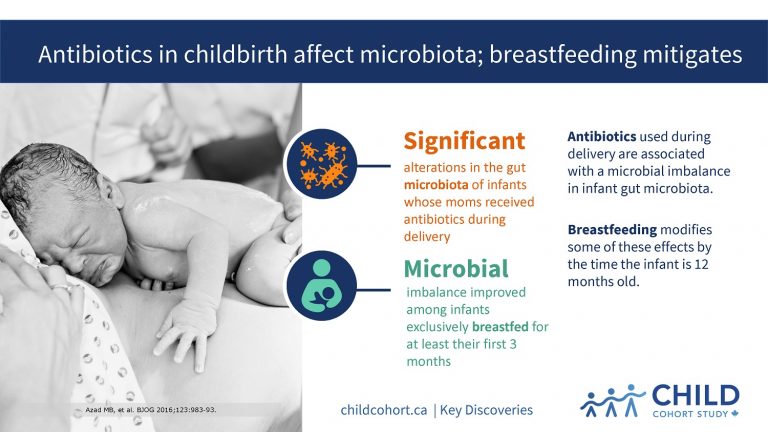
Antibiotics in childbirth affect microbiota; breastfeeding mitigates
CHILD research has found that antibiotics used during delivery—whether caesarean or vaginal—are associated with a microbial imbalance (or dysbiosis) in infant gut microbiota, and that breastfeeding modifies some of these effects by the time the infant is 12 months old.
“Antibiotics are commonly administered to mothers during birth to help protect infants from Group B Streptococcus (GBS) infection,” says the study’s senior author, Dr. Anita Kozyrskyj (University of Alberta).
DISRUPTION AT A CRITICAL TIME
“In North America, prophylactic antibiotics are given to all women with a positive vaginal culture for GBS, while some European countries base antibiotic treatment decisions on other risk factors.
“Our research provides evidence that exposing newborns to antibiotics disrupts their initial gut colonization at a critical time when a baby’s immune system is being established.”
Published in BJOG: An International Journal of Obstetrics and Gynaecology, the research examined data and samples from 198 healthy-term infants from CHILD.
Maternal antibiotic exposures during birth and birth method were documented from hospital records, and breastfeeding information was reported by mothers. The composition of the infant gut microbiota was characterised through the analysis of fecal samples taken at 3 and 12 months.
DNA sequencing techniques performed in the laboratories of James Scott, a co-Principal Investigator, and David Guttman at the University of Toronto provided information on the types and quantity of bacteria present in the infants’ stool.
A total of 43% of mothers received prophylactic antibiotics for GBS during delivery—21% during vaginal delivery; 13% during emergency caesarean-section; and 9% during elective caesarean-section—while 57% had a vaginal delivery with no antibiotics.
BREASTFEEDING REDUCES ADVERSE EFFECTS
At three months of age, infants born to women who received antibiotics during delivery had significant alterations in their microbiota, including a lower abundance of Bacteroidaceae and higher abundance of Clostridiales compared to infants whose mothers did not receive antibiotics. These differences persisted at 12 months of age among infants who were not exclusively breastfed for at least the first three months of life.
“Our findings provide new evidence that breastfeeding can modify antibiotic-induced microbiota changes,” says Dr. Meghan Azad, lead author of the study and Deputy Director of CHILD.
“Eventually, we hope to determine whether these antibiotic-induced changes in microbiota are associated with the development of obesity or allergic disease in children. We also plan to further explore how breastfeeding can minimize the adverse effects of antibiotic use, since there are times when it cannot be avoided.”
Read about this research in McLean’s Magazine.