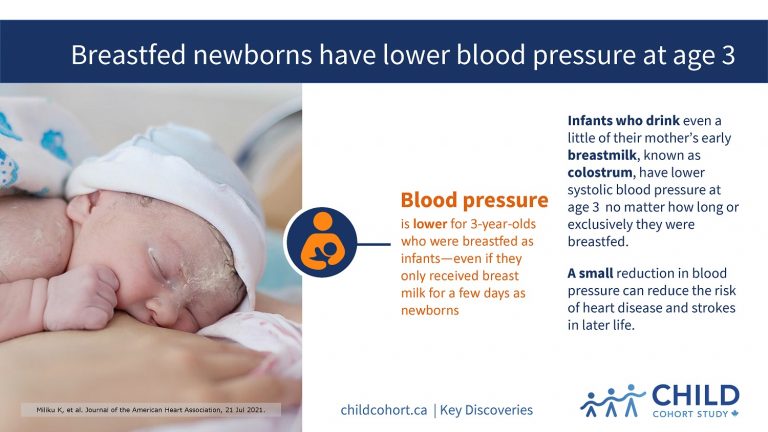
Breastfed newborns have lower blood pressure at age 3
Babies who are breastfed right after birth, even if only for a few days, have lower blood pressure at three years of age than children who were never breastfed.
CHILD research, published July 2021 in the Journal of the American Heart Association (JAHA), shows that infants who received even a relatively small amount of their mother’s early breast milk, also known as colostrum, had lower blood pressure at age three, regardless of how long or exclusively they were breastfed.
Colostrum contains immune, growth and tissue repair components that play a crucial role in building a child’s immune system.
“We know that breastfeeding is associated with lower cardiovascular disease risk in adulthood; however, the amount and length of time of breastfeeding needed to achieve this benefit has not been well understood,” said first-author Dr. Kozeta Miliku, a postdoctoral fellow at McMaster University and Clinical Science Officer for CHILD.
“To our knowledge, this study is the first to show the association of breastfeeding in the first days of life with blood pressure in early childhood.”
COMPARING DATA
The researchers analyzed infant feeding information collected from hospital records and caregiver questionnaires for nearly 2,400 children participating in CHILD.
These data were categorized relative to early-life breastfeeding as: none (no initiation of breastfeeding at all); “early limited breastfeeding” (limited to the hospital stay); or “sustained” (initiated and continued beyond the hospital stay). The researchers then compared the feeding information with the results of blood pressure tests taken when the children were three years of age.
They found that on average, compared to children that were never breastfed, those who were ever breastfed – even if they only received breast milk for a few days as newborns – had 3.5 mmHg lower systolic blood pressure at the age of three.
The researchers further found that associations between breastfeeding and child blood pressure were not explained by social, health or lifestyle differences between mothers, nor were they related to child body mass index.
EVERY DROP COUNTS
“Our results suggest that supporting breastfeeding initiation, even for a very brief period, could have a substantial impact on cardiovascular disease prevention later in life,” said senior author Dr. Meghan Azad, a Canada Research Chair in Developmental Origins of Chronic Disease at the University of Manitoba and Deputy Director of CHILD.
“It’s clear that ‘every drop counts,’ especially in the critical first few days of life.”
The research is especially relevant to hospitals implementing cost-containment strategies that could impede breastfeeding initiation, such as early postpartum discharge (often less than 24 hours following a vaginal delivery), and/or elimination of lactation support services on postpartum units, the authors suggest.
See Dr. Azad interviewed on CTV News about these findings
“There is also the added concern of the COVID-19 pandemic, as some mothers and babies were being discharged early from hospital – either as an infection control measure, or because hospitals were overwhelmed,” noted Dr. Azad, who also co-directs the Manitoba Interdisciplinary Lactation Centre (MILC) at the Children’s Hospital Research Institute of Manitoba (CHRIM).
“These moms may not have received the support they need to successfully establish breastfeeding. Ultimately, our hope is this research will help to inform and optimize infant feeding practices and promote programs and policies to support breastfeeding and improve a child’s long-term health.”